The condition develops with initial symptoms such as an inability to look up, an inability to look forward, a feeling of unsteadiness, and a stiff neck, and I think many people have never heard of the name “dropped neck syndrome”.
Dropped neck syndrome is caused by a decrease in the strength of the muscles that connect the neck to the back (the extensor muscles of the cervicothoracic transition).
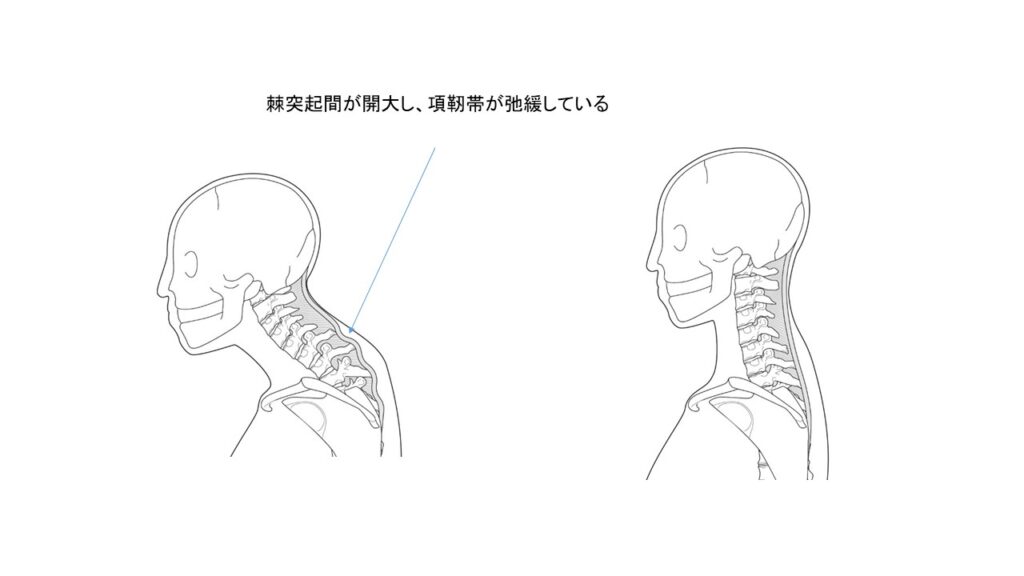
The muscles and ligaments (cervical ligaments) that support the cervical vertebrae become weak, causing the distance between the vertebrae to increase (intervertebral space).
It is “postural dysostosis,” a condition in which the patient is able to lift the head temporarily but is unable to maintain that position, and has been increasing in recent years as the population ages.
It may occur suddenly, but it starts with a feeling of discomfort like stiff shoulders, and since the symptoms are mild, it may be difficult to notice at first.
If diagnosed and treated at an early stage, the condition can be corrected, but if the condition persists for a long time, the muscles and ligaments become stretched and the condition deteriorates.
The neck drop is evaluated by CBVA (chin brow vertical angle), which is the angle between the facial tilt and the vertical line (normal value is within +/- 10 degrees in the x-ray below).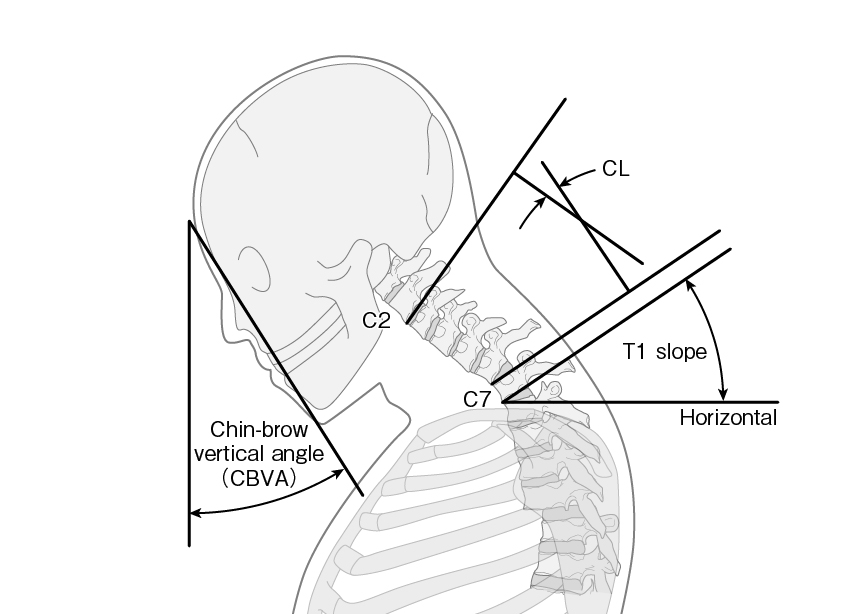
In the early stages of the X-ray classification of dropped neck syndrome, more than half of the patients do not have a drooping neck even when X-rays are taken. In the advanced stage, the neck droops by more than 10 degrees, and in the terminal stage, the patient is unable to look forward and has a chin-on-chest condition. The name of the disease, “neck-drop”, is not well known, and because early diagnosis is difficult, early treatment is often delayed. In order to make an early diagnosis of neck-drop, we have devised a questionnaire and neck-drop test. If you are a concerned, please try to do a self-diagnosis.

Sometimes you notice it only when someone else points it out to you, but gradually you start to feel that your head is getting heavier, so you bend forward, and when you force your head up, you feel a severe pain in your neck and back, but it goes away when you lie down. This type of condition can significantly reduce the quality of your daily life when you stand up. Some people find it difficult to walk with their head forward, and they also find it difficult to perform basic activities such as gargling, washing their face, brushing their teeth, swallowing food, and even breathing.
When you stand up, you will be hunched over because you are trying to lower your body backward with your hips to lift your head. You will also find it difficult to hold your head up when you walk.
It is important to check the cause, and it may be caused by cervical spondylosis due to aging, or by diseases of the nerves or muscles other than aging. The most important of these are Parkinson’s disease, dystonia (muscle spasms), and myopathy (a general term for diseases that cause muscle weakness). It is also necessary to be careful because the use of psychotropic drugs may have an effect.
The diagnosis is made by analyzing the state of muscle contraction using MRI, muscle biopsy (muscle tissue) and echo, as well as measuring blood samples, bone density and muscle mass.
If the neck (head) is left in a lowered position, the muscles will tear and be replaced by fibrous tissue, making it difficult to heal. For this reason, early diagnosis and treatment are important.
First, let’s try a self-diagnosis for neck sag.
– Does your neck hang?
You feel dizzy when you walk.
□ You can’t keep your head straight when you walk.
□ You have trouble doing things like gargling, eating, or reading.
□ You have difficulty with activities that require you to reach high places, such as hanging out the laundry.
You have trouble swallowing.
– There is a possibility that your drooping neck is caused by a neurological condition.
□ Your hands shake.
□ Your gait has become unsteady.
□ Your legs don’t lift when you walk.
□ Your back begins to bend
□ Memory loss becomes more frequent
It is difficult to diagnosis by myself.
Tension in the shoulders is sometimes the first symptom of a sagging neck.
Many people think it is just a case of stiff shoulders at first, but then their posture gradually worsens and they notice other people pointing out that their neck is drooping.
They are still able to do things around the house, but they find it more difficult to move around and their work becomes slower.
Tension in the shoulders → Drooping neck → Difficulty in daily activities → Difficulty moving around.
It is important to diagnose the cause as soon as possible and do the right rehabilitation exercises, rather than just taking medication or having a massage.
However, there are also cases where neck droop is caused by disease. If you have three or more of the symptoms listed in point 4, it may be caused by a disease of the brain or internal organs. Consult a neurologist or orthopedic surgeon.
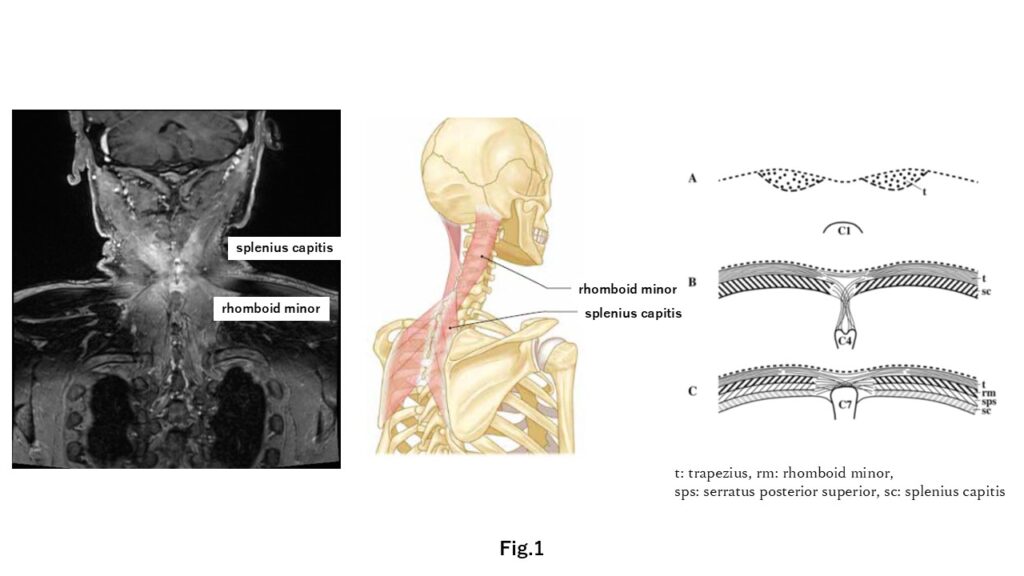
Recent our study showed contrast enhanced MRI is usuful for the diagnosis (Fig.1).
Endo, K., Nishimura, H., Sawaji, Y., Aihara, T., Suzuki, H., Konishi, T., … & Yamamoto, K. (2024). Contrast-enhanced Magnetic Resonance Imaging in Patients With Dropped Head Syndrome. Spine, 49(6), 385-389.
I usually propose self-exercise called “Kitty exercise” for avoiding cat like round back (thoracic kyphotic contructure).
-en-709x1024.jpg)
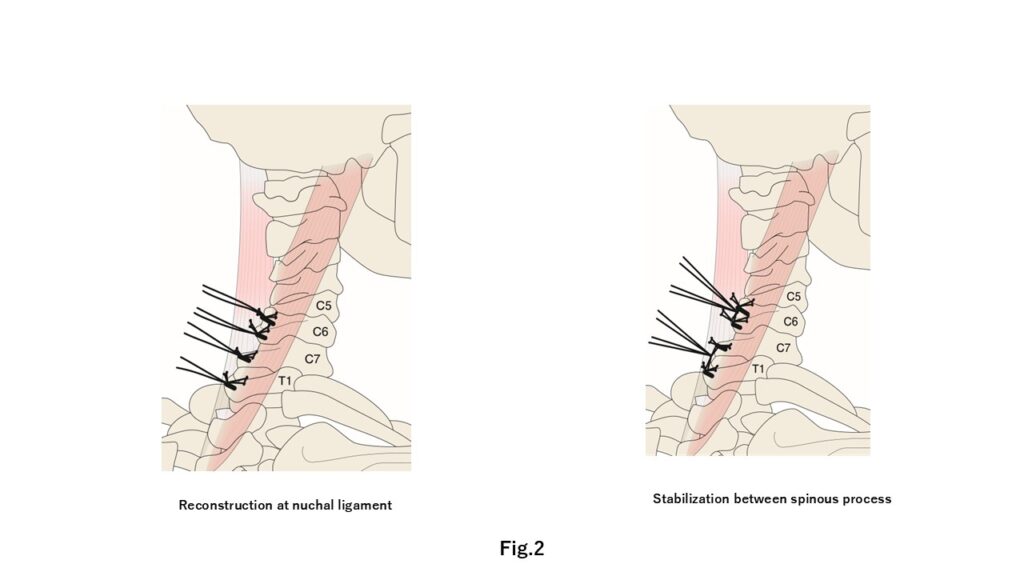
In case of non-respond conservative treatment, the operative treatment is one of choices.
However, the corrective fusion surgery for DHS would be an invasive procedure for elderly people.
We considered a novel fusionless nuchal ligament reconstruction & stabilization surgery (NLRS) for patients with dropped head syndrome (DHS) (Fig.2). We had experienced 45 cases, and the outcomes had been reasonable (CSRS-Europe 2025 @ Prague). Notably, the operative indication and rehabilitation before and after the reconstruction surgery would very important. When the operative indication and the rehabilitation were incomplete, the correction loss would be present large.
Endo K, Kanai H, Sawaji Y, Aihara T, Suzuki H, Konishi T, Nishimura H, Yamamoto K. Nuchal Ligament Reconstruction Surgery for Dropped Head Syndrome: A Case Report. JBJS Case Connect. 2024 Oct 18;14(4):e23.00611. doi: 10.2106/JBJS.CC.23.00611. PMID: 39423291; PMCID: PMC11486988.
Please read the following papers.
Endo K., Matsubayashi J, Sawaji Y., Murata K.,Konishi T., Nagao T. and Yamamoto K (2021).:Histological characteristics of cervical extensor muscle in patients with dropped head syndrome, Eur J Med Res. 2021 Nov 26;26(1):135.
Endo K, Kanai H, Sawaji Y, Aihara T, Suzuki H, Konishi T, Nishimura H, Yamamoto K. Nuchal Ligament Reconstruction Surgery for Dropped Head Syndrome: A Case Report. JBJS Case Connect. 2024 Oct 18;14(4):e23.00611. doi: 10.2106/JBJS.CC.23.00611. PMID: 39423291; PMCID: PMC11486988.
Endo, K., Kudo, Y., Suzuki, H., Aihara, T., Matsuoka, Y., Murata, K., … & Ishikawa, K. . Overview of dropped head syndrome (Combined survey report of three facilities). Journal of Orthopaedic Science, 24(6), 1033-1036.,2019.
Nishimura, H., Endo, K., Sawaji, Y., Suzuki, H., Aihara, T., Murata, K., … & Yamamoto, K. (2023). Global Sagittal Spinal Compensation for Dropped Head Alignment. Spine, 48(6), 421-427.
Sano H, Endo K, Sawaji Y, Aihara T, Suzuki H, Yamauchi T, Ishiyama M, Osada T, Ueno R, Masaoka T, Nishimura H, Yamamoto K. A novel diagnostic examination for dropped head syndrome (DHS) (Prone position cervical extension test; DHS test). J Orthop Sci. 2024 Sep;29(5):1179-1182. doi: 10.1016/j.jos.2023.09.003. Epub 2023 Oct 14. PMID: 37845161.
Murata K, Endo K, Suzuki H, Takamatsu T, Nishimura H, Matsuoka Y, Sawaji Y, Tanaka H, Yamamoto K.:Spinal Sagittal Alignment in Patients With Dropped Head Syndrome.Spine (Phila Pa 1976). 2018 Nov 1;43(21):E1267-E1273
Murata K., Endo K., Aihara T., Suzuki H., Matsuoka Y., Nishimura H.,Takamatsu T., Kusakabe T., Maekawa A., Uehara T., Yamamoto K:Relationship between cervical and global sagittal balance in patientswith dropped head syndrome, Eur Spine J 29, pages413–419 (2020)
Kusakabe T, Endo K, Sawaji Y, Suzuki H, Nishimura H, Matsuoka Y, Murata K, Takamatsu T, Maekawa A, Aihara T, Yamamoto K. Mode of dropped head syndrome and efficacy of conservative and efficacy of conservative treatment. J Orthop Surg (Hong Kong). Jan-Apr 2020;28(2):1-7. https://doi.org/10.1177/2309499020938882
Kudo Y, Toyone T, Endo K, Matsuoka Y, Okano I, Ishikawa K, Matsuoka A, Maruyama H, Yamamura R, Emori H, Tani S, Shirahata T, Hayakawa C, Hoshino Y, Ozawa T, Suzuki H, Aihara T, Murata K, Takamatsu T, Inagaki K. (2020). Impact of Spinopelvic sagittal alignment on the surgical outcomes of dropped head syndrome: a multi-center study. BMC Musculoskeletal Disorders, 21(1), 1-10.
Konishi, T., Endo, K., Aihara, T., Suzuki, H., Matsuoka, Y., Nishimura, H., … & Sawaji, Y. (2020). Global sagittal spinal alignment at cervical flexion in patients with dropped head syndrome. Journal of Orthopaedic Surgery, 28(3), 2309499020948266.
Endo K., Sawaji Y, Aihara T., Suzuki H., Matsuoka Y, Nishimura H, Takamatsu T, Konish T. and Yamamoto K (2021).:Eight cases of sudden onset dropped head syndrome ⎼ Illustrative cases, JNS lessons. (DOI link: https://doi.org/10.3171/CASE211771)
Qian, W., Endo, K., Aihara, T., Sawaji, Y., Suzuki, H., Matsuoka, Y., … & Yamamoto, K. (2021). Cervical sagittal alignment in patients with dropped head syndrome. Journal of Orthopaedic Surgery, 29(1), 2309499021990112.
Ueshima T, Endo K, Nishimura H, Sawaji Y, Suzuki H, Aihara T, Murata K, Konishi T, Kusakabe T, Yamauchi H, Matsubayashi J, Yamamoto K. Magnetic resonance imaging findings in patients with dropped head syndrome. J Orthop Sci. 2024 May 4:S0949-2658(24)00062-9. doi: 10.1016/j.jos.2024.04.005. Epub ahead of print. PMID: 38705766.